Did you know that there is an increasing number of claim denials in the industry?
A recent survey indicates that 54% of providers indicate that the number of denials is on the rise, and 41% say that at least one out of ten claims is initially denied. These delays limit payment, increase workloads, and may slow down the treatment of a patient. The CO-252 denial code is one of the guilty parties that show lack of documentation on a claim.
In this posting, we define the meaning of CO 252 in medical billing, the reason it occurs, and the method of correcting it. Other related denial codes that we discuss include PI-252, CO-22, MA-04, CO-97, and N479, and provide some practical tips that can assist practices to reduce denials, receive quicker payment, and optimize their revenue cycle. Providers Care Billing LLC has assisted hundreds of mid-size and small practices in overcoming denials through its custom-designed solutions.
What is the CO-252 denial code in Medical Billing?
The CO-252 denial code is a Contractual Obligation adjustment to indicate that the insurers require additional documentation before processing a claim. Simply stated, the payer is informing you of the fact that something very important is missing, such as clinical notes, lab results, or pre-authorization forms that demonstrate medical necessity.
CO in CO-252 represents Contractual Obligation. It implies that the provider was not able to comply with the documentation terms of the insurance contract. Practically, that tends to appear like a claim written in immaculate code and tossed out due to the absence of an important file.
One physical therapy clinic in Texas was filing claims for various sessions without attaching the modification of therapy evaluation forms. In the absence of such notes, the insurer had no opportunity to check medical necessity, hence the rejection of the claim with CO-252. The denial was to include the request that the missing reports be attached, and reimbursement should not proceed until the clinic compiled and sent the missing reports. This is an illustration of how the slightest paperwork break can be the trigger to CO-252.
Many practices across the U.S, including New York and Illinois, struggle with CO-252 denials due to missing documentation.
Common Reasons for CO-252 Denial Code
CO 252 rejections normally arise due to absence or incomplete information on the claim. The most usual causes are:
- Missing or Incomplete Attachments: The claim needed supporting documentation, such as medical records, labs, X-rays, authorizations, and the like, which were not provided.
- No or Incorrect Remark Code: The most frequent remark code is that insurers need a remark code to elaborate on the reasons why they need more information. In case of not using the right code or having the wrong formatting, CO-252 may occur.
- Insufficient Patient/Procedure Info: Critical information, including patient demographics, provider ID, or procedure codes, may be absent or mismatched.
- Lack of Medical Necessity Evidence: Records attached may fail to fully support the service. Failure to prove medical necessity leads to the issuance of CO-252 denials, as payers rely on medical necessity documentation standards outlined by CMS when reviewing claims for additional information.
- Unmet Payer Requirements: Special handling of some services is required prior authorizations, referrals, or forms are necessary. Inability to meet these triggers CO-252.
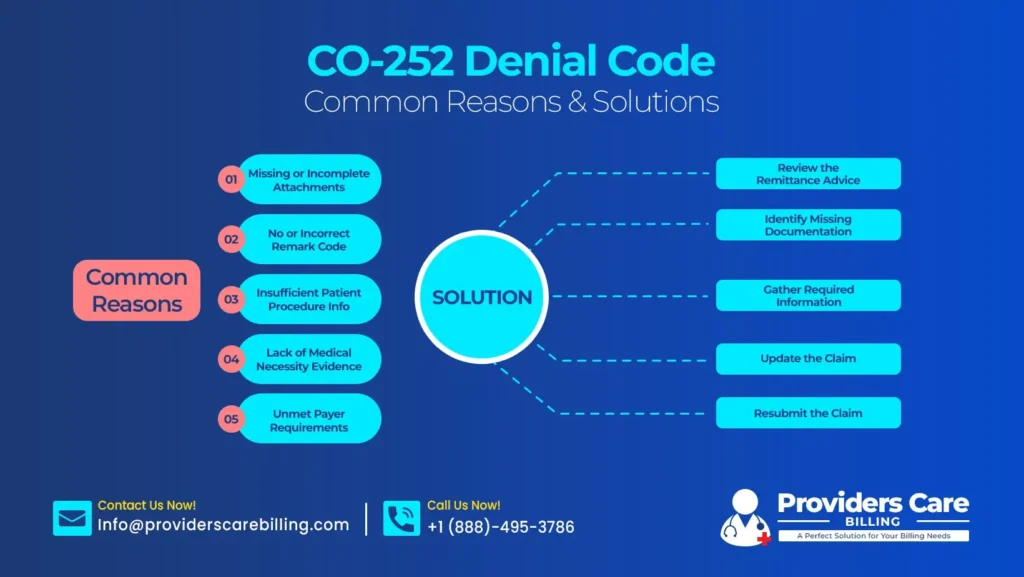
Proven Fixes: How to Resolve a Remark CO-252 Denial Code
A CO-252 denial is solved by a successive correction and resubmission:
- Review the Remittance Advice: Read the EOB carefully and take note of any remark codes or payer notes that identify what is not there.
- Identify Missing Documentation: Compare the rejected claim with your files and decide what documents or attachments must be submitted by the insurer.
- Gather Required Information: Approach the clinicians, laboratories, or departments to retrieve the lost clinical notes, test outcomes, physician notes, consent forms, or authorization letters.
- Update the Claim: Attach the missing documents and provide any necessary comments or rejection codes.
- Resubmit the Claim: Re-submit the revised claim to the payer. Including a cover note that points out the documentation added and any explanation.
- Monitor and Follow Up: Check on the resubmitted claim frequently, ensure receipt by the payer, and call the claims department when you do not get a response within a few weeks.
Best Practices to Prevent Denial Code CO-252 Before Submission
A pound of cure is worth an ounce of prevention. By following a structured approach to reduce claim denials in medical billing, practices can significantly minimize recurring CO-252 errors before claim submission. The following are industry best practices:
- Complete Documentation Checklists: Prepare comprehensive checklists of every type of service. Make a list of forms and records that are needed. Confirm every product before delivery.
- Standardize Remark Codes: Attach the correct remark codes to each claim. Apply billing software with automatic attachments of the non-alert RARCs in case of missing information.
- Staff Training: Keep your staff current on the documentation requirements of every payer. Front-desk and clinical staff are to be aware of gathering authorizations and patient records in advance.
- Claim Scrubbing Tools: Use claims management programs to identify missing attachments or invalid codes before submission. Omissions are detected in the edit stage by automated scrubbing.
- Internal Audits: Sampler Review of processed claims and denial reports once every so often. Detect trends and reassign tasks or retrain employees.
- Clear Communication with Payers: Keep the line open with payers. In case your team does not know what a certain insurer needs to be documented, you can call and ask, or you can check the provider manual of the payer.
Related Medical Billing Denial Codes to Know
CO-252 is not the only code that the providers are faced with. Some associated denial codes (which are usually used in conjunction with CO-252) and their significance are listed below:
- PI-252 (Patient Not Enrolled): It is a Patient-Initiated code. Attention was drawn by the insurance system to an eligibility problem. As an illustration, charging a patient the insurer of Group A, yet he or she is in plan B.
- CO-22 (Coordination of Benefits): means that the primary insurer was forwarded the claim. As an example, CO-22 is activated by the billing of Medicare as primary despite the patient having active employer insurance.
- CO-253 (Sequestration): a Medicare-specific modification. CO 253 signifies that the payment has been decreased by federal sequestration, which is at present 2 percent reduction on Medicare payments.
- MA-04 (Medicare Secondary Payer): associated with Medicare being billed as secondary. You are required to include an EOB of the main insurer. In its absence, the claim can be denied or suspended by Medicare.
- M127 (Missing Medical Record): typically comes with a CO-50 or denial CO-59. It is a sign that the payer ordered medical records that were not made available. Locate the missing notes and return.
- CO-97 (Billed Service/Non-Payable): is used to indicate that the service is not charged individually. Charging out a minor service on its own when it is part of a global fee for a major surgery is a kind of CO-97 trigger.
- N479 (Missing EOB to Secondary): happens when the primary payer EOB is not included with the billing of a secondary insurer. This is a compulsory formality for COB claims.
- Other Common Codes: CO-16, CO-50, CO-197, etc. As an illustration, CO-197 implies that a pre-authorization or certification process was not carried out.
Ready to get rid of CO-252 denials and increase revenue? Work with Providers Care Billing LLC and receive payments sooner and fewer complaints related to billing. Book a FREE consultation appointment now and learn how our tailored billing platforms can change your revenue cycle.
How Providers Care Billing LLC Helps (4.9-Star Denial Experts)
Dealing with CO 252 and other codes of denial may overwhelm a busy practice. That is where an experienced billing partner, such as Providers Care Billing LLC, will come in. Our team offers:
Specialized Experience
We have solved thousands of refusals CO-252 and PI-252 problems. Our coders and billers are familiar with the payer regulations and are often so acquainted with them that they know what is going to be declined before submitting claims. This has been proactive in ensuring that we claim client satisfaction more than 99 percent. Denial rates have reduced to single figures among many clients.
Customized Solutions
Every practice is unique. We custom fit workflows to match your specialty. Mental health providers require different documentation than orthopedics, e.g. To prevent the problem of CO 252 at its origin, we tailor denial scrubbing rules and training to prevent the problem.
Advanced Technology
We have certified RCM software that identifies absent attachments, invalid codes, or eligibility issues. Notifications are made prior to the claims being forwarded. In case of a pre-auth, our system will not release a claim without a reminder.
Dedicated Follow‑Up
In case of CO-252 or other denials, our Denials Management team intervenes immediately. We refile claims, contact payers (frequently faster than practices can), and keep you posted. In a success case, a dental practice reduced its denials by 50 percent in two months of our intervention (CO 252).
Transparent Partnership
Providers Care provides complete visibility. Our portal is safe, and it allows you to monitor the status of claims, denials, and appeals. We also provide free consultations and denial reports; therefore, you are always aware of your status.
Conclusion
Such denials of claims as CO 252 must never become a sort of a long lasting bottleneck. Knowing all the codes and best practices, you will be able to increase the cash flow significantly. According to one of the billing managers, working with Providers Care changed our revenue cycle; denials decreased, and we finally received payments on services we are providing.
Want to see similar results? Get a free consultation with Providers Care Billing LLC. Your denial problems will be looked into by our professional team and will streamline your billing process and help you recover every dollar that your practice is entitled to. We have established low service rates and a promise of customized service; we will make billing an easy, correct, and lucrative task. No more lost income on the lost attachments and the not so obvious codes. Call us now and convert those refusals into dollars.
Frequently Asked Questions
What causes a CO-252 denial, and how do I remedy it?
CO-252 is in instances where documentation is still wanting or incomplete. Find out the missing items, get the required files, and file a claim again with those attachments and any comments or codes that are relevant.
What can I do to avoid CO-252 denials in the first place?
Prevention is dependent on detailed documentation. Prevent gaps with the use of checklists and training. Ascertain that all supporting documents are attached, flagging omissions with claim-edit software, and checking upfront authorizations and referrals.
What are the CO‑22 and CO‑253 codes?
The typical CARC/remark codes are:
- CO -22: Coordination of Benefits the claim was sent to the primary payer incorrectly. First of all, resubmit to the right insurer.
- CO-253: sequestration, a mandatory reduction in Medicare of 2 percent; no mistake.
What should I do to get expert assistance in case of such denials?
Never argue with rejections. Providers Care Billing LLC provides a complimentary review of your denial issues. Your EOBs (including CO-252s and other codes) will be reviewed by our specialists, and specific recommendations will be made.