Tired of complex billing procedures? Look no further than Providers Care Billing, your one-stop shop for outstanding medical billing services tailored to your specific needs – all at the most competitive prices.
As a premier medical billing company, our expert team ensures that every medical procedure, test, and treatment is accurately translated into codes that insurance companies understand. This precision means fewer claim rejections and faster payments for you with our top-notch medical billing services.

Unique solution for your medical billing services that guarantees 100% correct claims submission. As a leading medical billing company, we offer a 99% FTPR, complete revenue cycle management services including medical billing, coding, credentialing, and enrollment.
Our timely claims submission, denial management, fixing rejections, and follow-up make the whole billing process very smooth. Our HIPAA-certified medical billers and HIPAA-compliant tools ensure the highest standards of security and privacy.

Our comprehensive medical billing services are here to make a real difference. Say goodbye to mere account monitoring – we proactively take charge of your accounts. With our experienced team of medical billing professionals, you get more than simply a service – you get a dedicated offsite billing department.
Our top-notch team ensures you receive the maximum reimbursement with our specialized medical billing expertise. Let us handle your billing worries while you focus on what truly matters – providing excellent patient care. Choose smart, efficient, and effective management with our trusted medical billing company.
Providers Care Billing LLC understands the complexities of medical billing can be overwhelming. That’s why we’re here to simplify the process for you!

To avoid surprises down the line, our team rigorously examines benefits and eligibility.
Accurate billing starts here. We ensure that every service is correctly documented and translated into charges.
Our rigorous editing and auditing process minimizes errors and ensures speedy claims processing.
We submit electronic and paper claims within 1 business day of receiving them.
To ensure treatments are covered from the start.
Expect dedicated follow-up within 7 days to keep claims moving smoothly.
Our certified coders ensure ICD-10 compliance, avoiding unnecessary hiccups.
We handle payment posting and adjustments with precision.
Our patient call center responds to inquiries professionally and compassionately.
Our collection strategies ensure your finances remain strong.
We manage accounts receivable to keep your practice's financials in check.
We assist clinicians and individuals in comprehending the Explanation of Benefits (EOBs).
We manage secondary and tertiary claims submissions, optimizing your revenue potential.
Medical Coding complexities shouldn’t hold your practice back.
As a leading medical billing and coding company, we offer top-tier medical coding services to meet all your needs. Our Certified Coders ensure seamless and error-free coding with a deep mastery of CPT Category I & Category II, and ICD-10, we guarantee utmost accuracy and compliance in every medical coding assignment.
Say goodbye to potential coding issues – we’re here to catch and fix them. Trust us to assign the most precise codes for the services you provide – always in sync with AMA and CMS guidelines.
Struggling with denied medical claims? We understand the frustration when your hard work goes unrewarded due to technicalities. We also know that manually managing these denials is like navigating a maze blindfolded – time-consuming and costly. The Medical Group Management Association (MGMA) reports that managing the average denial can cost between $25 to $30!
So, how do we turn this around? Our strategy is clear-cut and efficient. We dig deep to uncover the root causes of these denials. We leave no stone unturned in figuring out the technicalities that lead to rejections. And then, armed with this knowledge, we work on minimizing those denials and improving your practice’s collections.
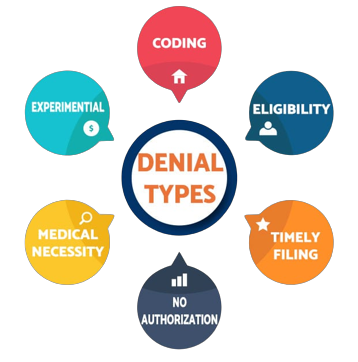
We meticulously check each claim in real time, verifying the CPT and ICD codes. We make sure they align with payer guidelines, reducing the chances of errors and delays.
Navigating payer rules can be daunting, but not with us by your side. Our advanced rules engine keeps a vigilant eye on payer denial trends and updates.
Transparency is vital in the billing process. Our automated alerts keep you in the loop about claim re-submissions and statuses.
Our customized reports provide real-time insights into your medical billing landscape. We make sure your claims are paid in full and identify areas for enhancement. It's about maximizing your revenue while continuously improving.

Connecting with insurance networks can be a complex task, but with Providers Care Billing LLC, it’s a piece of cake! Our service is all about making things easy for you. When you partner with us, you won’t need to worry about the nitty-gritty details. We’ll take care of the hard work, like analyzing your fee schedules and keeping a constant eye on your application status.



Providers Care Billing LLC is a leading medical billing services company, specializing in comprehensive revenue cycle management for healthcare providers across the USA. We are committed to delivering cost-effective, reliable billing solutions. Contact us today for a free consultation and discover our industry-leading healthcare billing services.
© 2025 Providers Care Billing LLC | All Rights Reserved