Did you know that in every three medical claims, one is rejected?
In the U.S. healthcare system, the cost of claim denials has reached billions of dollars annually. According to industry statistics, a significant number of denials are due to avoidable errors: wrong coding, missing modifiers, eligibility issues, or just data entry errors. The positive point is that claim scrubbing in medical billing is able to reduce denials by 70-80 percent.
We are Providers Care Billing LLC, a USA based medical billing company providing services across states like New York, California, and Texas. We focus on enhancing healthcare claims. This is done using advanced claim scrubbing software, professional coding review, and denial prevention techniques. We will explain in this complete guide:
- What is claim scrubbing
- The effect of scrubbing in medical billing.
- The position of a medical claim scrubber.
- Clean claims in medical billing: how to.
- The way your practice is able to increase revenue by smarter claims scrubbing.
What Is Claim Scrubbing in Medical Billing?
In case you are in doubt about what claim scrubbing is, then here is the easy solution:
Claim scrubbing is the procedure of examining medical claims to identify errors and submitting them to insurance payers. It ensures that claims are compliant with payer standards, coding requirements, and regulatory standards.
What is data scrubbing?
Data scrubbing refers to the process of correcting or removing poor or incomplete data. This is the same thing in healthcare billing, where claims undergo the procedure to verify their accuracy prior to their submission.
What Is Claims Editing?
Another question many providers have is, what is claims editing?
Claims editing is included in the scrubbing process. Rules-based systems compare each claim to payer policies, National Correct Coding Initiative (NCCI) edits, and medical necessity rules. Consider it as a review layer within your claim scrubber that is automated.
Why Claim Scrubbing in Medical Billing Is Essential
Contemporary claims management relies on compliance and automation. As CPT codes are updated frequently, ICD-10 codes, HCPS codes, CMS guidelines, and payer-specific policies are updated, manual review is no longer sufficient.
Medical billing can be assisted by proper scrubbing to aid in:
- Claim denial prevention
- Faster reimbursements
- Improved compliance
- Reduced rework costs
- Better cash flow stability
Your revenue cycle is insecure in the absence of effective claim scrubbing.
How Claim Scrubbing Works
A successful claim scrubbing process in medical billing involves a systematic process of reviewing that reveals errors before claims are submitted to the payer. Professional claims scrubbing works in the following way:
Accurate Data Capture
This begins by using full and correct patient and service information in the billing system. This contains patient demographics, insurance details, provider details, date of service, and cpt, icd 10, and hcp codes to be used. Any minor coding errors or lack of data at this stage is liable to create future issues, hence it must be accurate.
Review of Automated Claim Scrubber
The next step is that the claim is run through sophisticated scrubber software, which automatically reviews invalid or old codes, NCCI edits, bundling, missing modifiers, payer-specific requirements, and duplicate submissions. This is an automated layer that is paramount in avoiding denials, and claims are managed effectively.
Code Check and Claims Editing
At this stage, the scrubber ensures that the procedure codes are supported by diagnosis codes. It uses rule-based validation to implement accuracy in coding and compliance with medical necessity. Correct scrubbing involves no mismatched pairs of diagnosis and procedure, accuracy of modifiers, and claims that do not exceed the payer limits, which is the most important aspect of clean claims.
Eligibility and Authorization Check
The system checks active insurance coverage, previous-authorization requirement, referral compliance, and coordination of benefits where applicable before submission. Numerous refusal cases are caused by eligibility or authorization loopholes, which is why this step is paramount.
Final Review and Submission of Quality
The claim is finally subjected to a quality check once all the issues that have been flagged are resolved. After being validated, it is transmitted electronically to the clearinghouse and payer. The outcome is an increase in first-pass acceptance rates, a reduction in rejections, and an increase in cash flow.
Common Medical Coding Errors Detected During Claim Scrubbing
Proper scrubbing of claims will help determine problems before it results in denials.
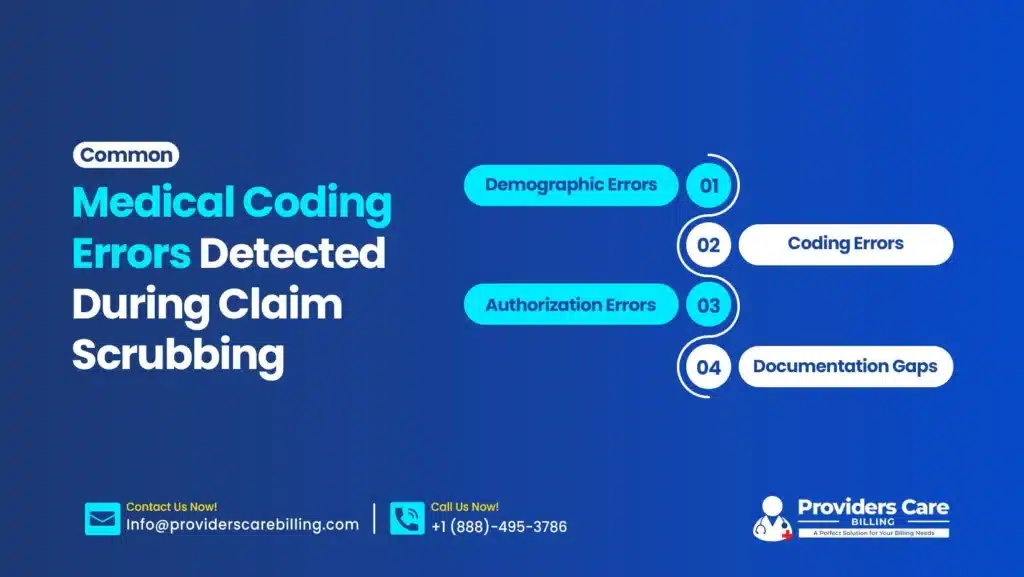
1. Demographic Errors
- Misspelled patient names
- Incorrect date of birth
- Use of wrong insurance identification numbers.
2. Coding Errors
- Outdated ICD‑10 codes
- Incorrect CPT selection
- Missing modifiers
- Non-supportive diagnoses of medical necessity.
3. Authorization Errors
- Lack of previous approval.
- Expired referrals
- Non‑covered services
4. Documentation Gaps
- Lack of sufficient documentation.
- Missing provider signature
- Incomplete encounter notes
Such medical coding mistakes have been the leading cause of claim denials in the country.
The Role of Claim Scrubbing in Claims Management in Healthcare
Successful claims management within healthcare is based on prevention rather than correction. The lack of proper claims scrubbing results in the following practices: An active claim scrubber is one that guarantees a correct claim the first time.
- Increased denial rates
- Cash‑flow interruptions
- Compliance risks
- Lower profitability
Future Trends in Claim Scrubbing
Healthcare billing has been developing. Key trends include:
- Claim scrubber software, based on AI.
- Predictive denial analytics.
- Automation of prior-authorization checks.
- Improved compliance check software.
- Live payer policy integration.
Providers Care Billing LLC keeps up with the changes in CMS updates and changes in codes and billing to defend your revenue.
Why Choose Providers Care Billing LLC?
We are a U.S.A. based medical billing company that focuses on the optimization of the revenue cycle of:
- Private practices
- Specialty clinics
- Multi‑provider groups
- Behavioral health providers.
- Primary care practices
Our services include:
- Full scrubbing of claims in medical bills.
- Denial management
- Medical coding audits
- Credentialing services
- Revenue cycle management
- Compliance monitoring
- EHR integration support
We emphasize providing clean claims to enhance financial resilience and regulation.
Stop losing business to avoidable rejects. Collaborate with Providers Care Billing LLC and enjoy smarter claim scrubbing, reduced denial rates, and quicker reimbursement.
Contact us now and receive a Free Revenue cycle evaluation and learn how our professional medical claim scrubber services can enhance the financial results of your practice.
Final Thoughts
Claim scrubbing in medical billing is not only necessary, but it is an obligatory part of a complex billing environment today. As the coding updates and payer policies alter incredibly fast, one will require a solid claim scrubber software and expert supervision in order to secure revenue. Providers Care Billing LLC provides superior claims scrubbing, denial prevention, and full claims management to help your practice to flourish. Turn your billing problems into financial improvement.
FAQs
What is the effect of claim scrubber software on denials?
The software identifies and reports coding errors, absence of information, and eligibility issues before the submission. It allows claims to be cleaner and reduces the rework and denied claims by preventing them early.
Are all denials prevented by scrubbing claims?
Scrubbing will reduce the denial rate by a very large amount, but it cannot eradicate all denials. There are certain denials that occur due to changes in the payer policies or the coverage limit beyond the scope of billing.
What is the significance of scrubbing in medical billing as far as revenue cycle management is concerned?
Scrubbing increases the chances of claiming and approval on the initial attempt, enhances the speed of reimbursement, and improves the general management of claims. It eventually secures and boosts practice revenue.