Did you not learn that medical billing mistakes make U.S. healthcare providers spend over 125 billion dollars annually? The partner selection can be the difference between clean claims, quicker reimbursements, and increased revenues, and months of lost revenues and denials. When it comes to picking the best medical billing company USA, you are not the only one wondering how to do it. Most of the practices fail to find a reliable partner who can accommodate the insurance claim processing services, denial management services, and optimization of the revenue cycle.
We have assisted practices in the U.S. to simplify medical billing and coding outsourcing, enhance collections, and remain up-to-date with the regulations in the present day. We dissect all the information you have to know to choose the best medical billing companies in the USA in this 2026 guide.
Step 1: Have a Vision of Your Practice
Practice Assess your practice needs:
- Specialty: There are those that are behavioral health, orthopedic, or a multi-specialty firm.
- Claim volume: High-volume practices should be automated.
- Services required: Determine whether you require denial management, credentialing, or complete-service revenue cycle management.
- Location: There are those who like regional support, such as a billing service in California or a provider in New York.
Spinning off what you want helps to reduce the number of prospective outsourcing firms.
Step 2: Find Experience and Certifications
Experience matters. The partner who has been dealing with similar practices will take care of the coding complexities in a more effective manner. Examine certifications, including:
- Certified Professional Biller.
- Certified Professional Coder.
Depending on your specialty, the most accepted certification is CPC and CPB in the U.S. More partners are experienced, which helps to minimize mistakes, claims rejection, and simplify the process.
Step 3: Test Technology and Software
Modern billing in the medical field is dependent on technology. Look for firms that offer:
- Built-in billing software, e.g., Vision or other systems.
- Insurance claims secure portals.
- Automated denial control.
- Reporting dashboards in real-time.
A technologically advanced partner provides quicker reimbursements and visibility of the claims.
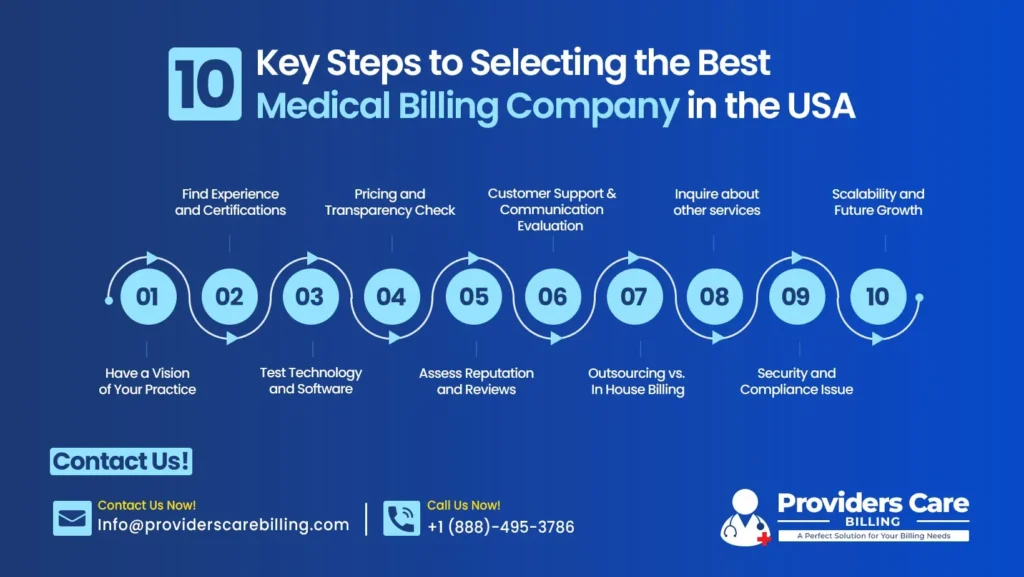
Step 4: Pricing and Transparency Check
There are varying rates based on services, volume, and complexity. Typical structures include:
- A collection rate. (5-10% average in the U.S.)
- Flat monthly fees.
- Hybrid models.
Inquire about any concealed expenses and extra charges on credentialing, denial appeals, and other services.
Step 5: Assess Reputation and Reviews
Online research literature and request. Find companies that have a good track record, i.e.:
- New York billing companies are renowned for being accurate.
- California identified efficient services.
Success stories of denial management and revenue growth are testimonials that will assure you of quality.
Step 6: Customer Support and Communication Evaluation
Billing errors happen. A company to be responsive should include:
- Dedicated account managers.
- Fast settlement of claims rejections.
- Frequent reports and consultations.
- Reflective practice development.
Effective communication keeps you updated and ensures claims accuracy. For more insights, read our blog on common medical billing claim denials.
Step 7 – Outsourcing vs. In‑House Billing
The comparison of medical billing outsourcing firms in the USA with the in-house team is done in many ways. Outsourcing has the following advantages:
- Lower overhead costs.
- Availability of qualified billing personnel.
- Improved denial management services.
- Increased adherence to shifting regulations.
Coming to the reputable Medical Coding Company will allow your practice to concentrate on patient care and maximize its revenue. Read our detailed guide on outsourcing vs in-house medical billing for small vs large practices.
Step 8 – Inquire about other services
The top medical billing firms in the USA do not only provide basic billing. Look for:
- Denial‑management services.
- Credentialing and insurance enrollment: This task involves having a nurse credentialed and enrolled in insurance coverage to qualify for Medicaid.
- The services include: revenue-cycle management.
- Marketing assistance- medical-billing marketing to lure new customers.
Selecting a full-service partner will provide success in the long term.
Step 9 – Security and Compliance Issue
HIPAA compliance is not something that can be compromised when it comes to the insurance claims and the data about patients. Look for:
- Secure cloud storage.
- Data transfer that is HIPAA compliant.
- Audiomedical-billing services audited.
- Open medical billing and medical coding outsourcing policies.
An insured patient and practice are safeguarded by a secure partner.
Step 10 – Scalability and Future Growth
A medical billing partner ought to support the expansion of the practice. Ask:
- Are they able to perform multi-location billing?
- Do they offer real-time reporting in growth analysis?
- Does it fit with your Revenue Cycle Management Services/Company?
Scalable services allow you not to change billing partners when your practice grows.
The increase in revenues by a Billing Partner
A New York multi-specialty clinic had problems with delayed payment and elevated denial rates. Having collaborated with a more established medical billing company USA, they:
- Reduced claim denials by 40%.
- Cut AR days from 60 to 35.
- Enhanced general cash flow in three months.
This is one of the reasons why it is essential to select the most competent medical billing provider.
Are you willing to increase your practice income and simplify billing? Collaborate with a major-medical billing firm to manage the claims, rejections, and coding with accuracy. Have a free consultation with us today.
Conclusion
The selection of the most effective medical billing firms in the USA must be conducted with a critical consideration of experience, technology, price, compliance, and services. A good medical billing partner will enhance the cash flow, minimize the denials, and enable your practice to concentrate on patient care. Whether it is insurance claim processing or even denial-management services, the choice of the provider is a long-term investment in the development of your practice.
Providers Care Billing LLC is an organization that provides medical billing, coding, credentialing, and revenue-cycle management services. We assist practices that focus on efficiency, accuracy, and full-service solutions.
FAQs
What are the actual criteria for selecting a medical billing company USA?
Analyze experience, technology, qualifications, cost, and reputation. Make service customers for your practice.
What services are supposed to be offered by the best medical billing services?
Search insurance claim processing, denial-management services, credentialing, reporting, and revenue-cycle management.
To outsource or to hire? Medical billing.
Outsourcing provides cost reduction, experience, and scalability. In-house can be used in small practices with low claims.
What is the best certification for medical billing?
The most widely used certifications in the U.S. are the following :
- Certified Professional Biller.
- Certified Professional Coder.