CPT code 96136 and 96137 are necessary for billing the time spent administering psychological and neuropsychological tests. They enable clinical psychologists and physicians to document and be paid for ADHD testing via CPT code, cognitive evaluations, and other mental health assessments. This article explains CPT codes for psychological testing, their application, as well as billing errors management.
CPT Code Background: Why 96136 & 96137 Exist
In 2019, CMS revised psychological testing codes to increase clarity and better align with the clinician’s workflow. In the past, test administration, scoring, and interpretation were grouped under limited codes, which created a lot of chaos.
With new revisions, additional time-based codes were created. 96136 and 96137 specifically address the test administration and scoring done by a licensed provider as opposed to a technician. Also, 96130 and 96131 were designated for interpretation and reporting.
This change assists both providers and payers in distinguishing between time spent collecting data and analyzing the data.
CPT 96136: Understanding the Core Code
Definition:
The 96136 CPT code is involved with the administration and scoring of tests done by a licensed professional for the first 30 minutes.
· Minimum time requirement: 16 minutes
· Who can bill it: Psychologists, physicians, nurse practitioners, or other licensed providers.
· Setting: Outpatient clinics, hospitals, private practices.
Clinical scenarios
· Administering the MoCA or MMSE in a dementia evaluation.
· Conducting cognitive testing for adult ADHD.
Documentation Essentials
· Exact name of tests (e.g., WAIS-IV, Trail Making Test).
· Total time spent (e.g., Administered and scored tests over 28 minutes).
· Patient diagnosis and rationale (e.g., mild cognitive impairment or suspected ADHD).
This code must be used first before adding the 96137 CPT code.
CPT 96137: Add-On Code Explained
CPT 96137 is an add-on code. This code is used for each extra 30 minutes of test administration beyond the first half hour.
· Must follow: 96136
· Cannot stand alone
· Used by: Same providers eligible for 96136
Example
A neuropsychologist administers the WAIS-IV, WMS, and Stroop Test in 90 minutes total. You bill 96136 (first 30 minutes) and 96137 x 2 (next 60 minutes).
Documentation Tips
· Break time into blocks: First 30 min: WAIS-IV; Next 30 min: WMS; Last 30 min: Stroop.
· Specify which tests were used in each time segment.
· Include a total time tally
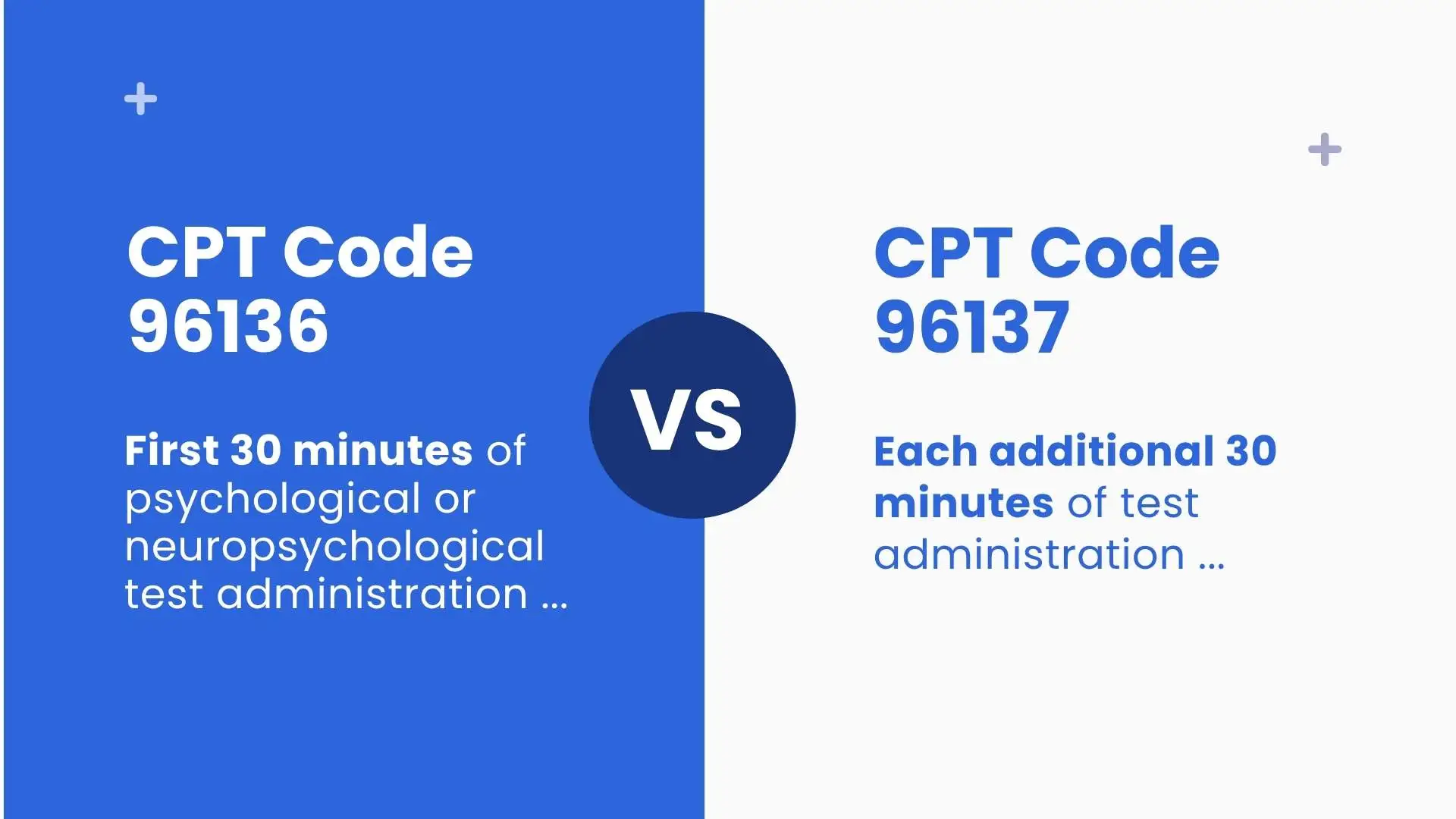
Comparison: CPT Code 96136 and 96137
| Feature | 96136 | 96137 |
| Time Block | First 30 minutes | Each additional 30 minutes |
| Code Type | Standalone | Add-on |
| Who Performs | Physician or qualified professional | Same |
| Minimum Time | 16 min | 16 min for each additional 30 min |
| When to Use | Always first | Only if testing exceeds 30 minutes |
Real-World Use Cases
Use Case 1: Short ADHD Evaluation
· A psychologist spends 28 minutes administering a test battery for suspected ADHD.
· Bill: CPT code 96136 only. Because the time didn’t exceed 30 minutes.
Use Case 2: Extended Cognitive Assessment
· 70 minutes spent on memory loss assessment.
· Bill: 96136 + 96137 x 1.
· 30+30+10, we can’t bill 96137 x 2 because for 3rd interval time didn’t reach its minimum limit of 16 minutes.
Use Case 3: Technician-Administered
If a technician performs the testing under supervision, use 96138/96139 instead of 96136/96137. Because these codes are only used when a licensed provider, Psychologists, and physicians perform the test.
Use Case 4: Multi-Day Testing
For testing procedures conducted over several days, start each day with 96136.
Documentation & Audit Readiness
Audit-proof documentation is essential. For good documentation, consider including the following:
· Total time spent (with breakdown)
· Specific tests administered
· Clinical rationale/diagnosis
· Provider credentials
Sample Note:
Administered the WAIS-IV and WMS over 75 minutes. Scored tests during the session. Testing indicated deficits consistent with mild cognitive impairment.
Common Diagnoses:
· F90.0 ADHD
· F81.0 Reading disorder
· G31.84 Mild cognitive impairment
Avoiding Coding Errors
Top Mistakes
· Billing 96137 without a prior 96136.
· Using 96136 for technician time (use 96138 instead)
· Rounding up incorrectly — only do so after 16 minutes
· Not documenting medical necessity or tests performed.
Pro Tip: To ensure compliant documentation, create templates in your EHR system.
Advice on Insurance and Reimbursement
Medicare:
· Accepts both codes.
· Time and clinical necessity must be documented.
Medicaid:
· Policies are state-specific.
· Psychological testing pre-authorization may be required for some.
Commercial Payers:
· Check coverage with the credentialing provider.
· See 96137 modifier 99214 or similar bundling rule applicability.
· Always link the appropriate ICD-10 code and submit accurate unit calculations.
Recommended Actions and Provider Suggestions
· Use a stopwatch or EHR timer to note the accurate time
· Maintain a document containing commonly performed tests and their duration.
· Conduct staff training on the appropriate usage of CPT code 96136 versus 96138 (for technician use).
· Review policies from payers every three months.
· Perform internal audits to assess compliance with coding guidelines.
Understanding Modifiers for 96136 and 96137
Modifiers are particularly important for proper payment and avoidance of denials when billing for 96136 and 96137. Although these codes do not always require modifiers, certain Medicare and private insurance payers often request them based on the service rendered or the setting.
Common modifiers are:
· Modifier 95: Use when the service telehealth is rendered (if permissible).
· Modifier 25: Sometimes necessary when psychological testing is done on the same day as an E/M service.
· Modifier 59: Applicable to differentiate testing services from other procedures where there is a risk of bundling.
All healthcare providers must verify each payer’s specific guidance regarding whether a modifier, if any, is required. Improper use of modifiers may result in claim denials or post-payment audits.
When conducting psychological or neuropsychological assessments, it’s important to consider any coexisting conditions that may impact mental health or cognitive function. For instance, metabolic disorders like pure hypercholesterolemia (ICD-10-CM Code E78.00) can be relevant in comprehensive patient evaluations. Learn more about E78.00 here.
Conclusion
The 96136 CPT code and 96137 CPT code enable providers to bill accurately for the test administration and scoring services. Providers need to understand the differences between 96136 vs 96137 documents succinctly, steer clear of common errors, and strive for compliance and appropriate payment.
Whether from ADHD testing CPT code or screening for dementia, these codes are pivotal in effective patient care and the sustainability of your practice. If used correctly, CPT codes for ADD and other assessments become integrated into the clinical workflow. For sustainable success, coordinate your coding with payer reimbursements.
Consulting billing professionals can help you better understand these codes and ensure you receive your reimbursement on time. These professionals are well-trained in using CPT codes and always update their knowledge and learn about new policies.