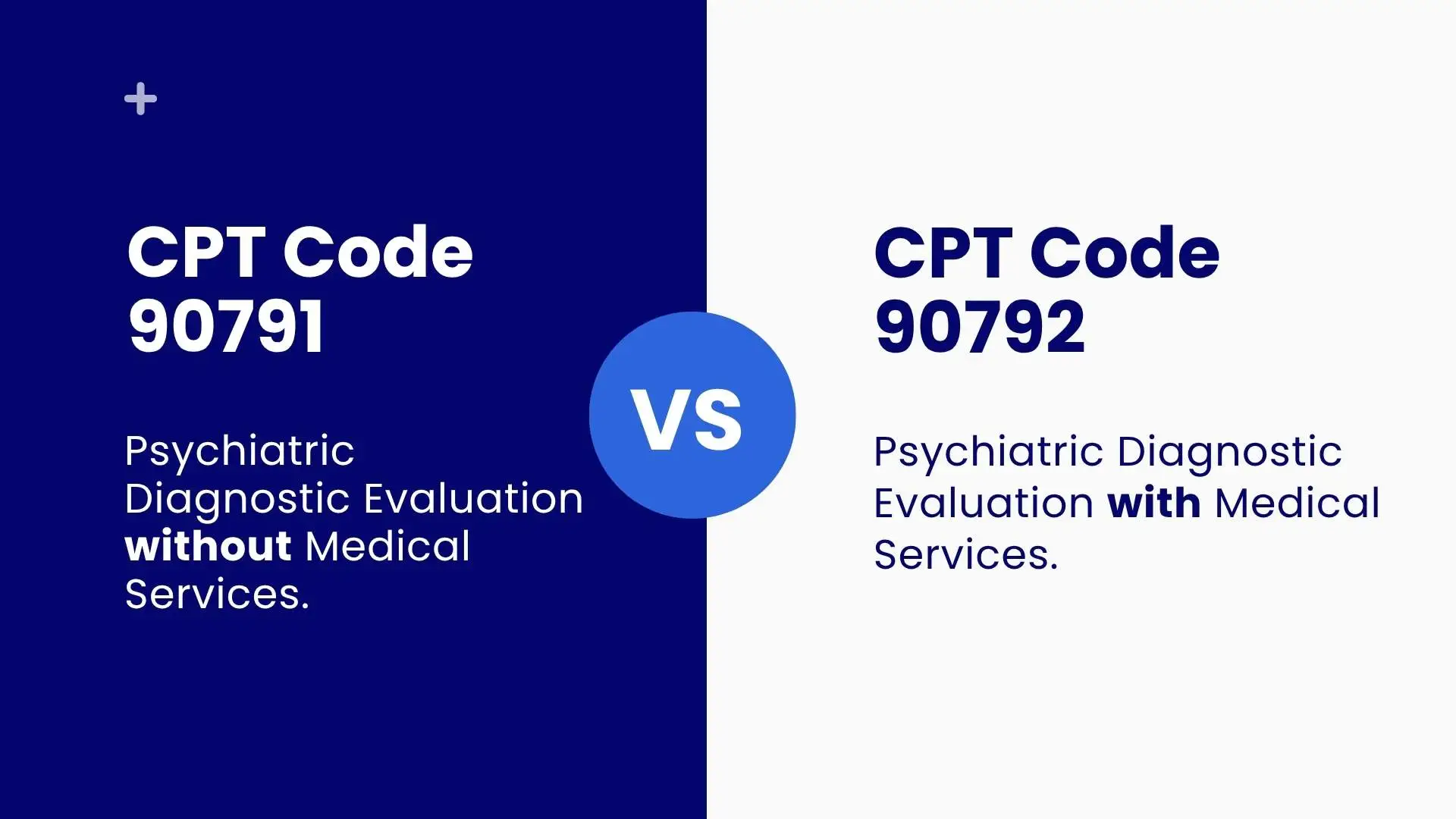
Two specific codes commonly arise in the realm of psychiatric facilities are 90791 and 90792. Both of these codes are relevant in psych evals, but they differ in terms of who can provide them, what services can be provided under them, and payment differences. Without these distinctions, billing and patient care won’t be optimized.
This document analyzes the difference between 90791 and 90792 as well as time commitments necessary for these procedures, payment grade details, and auxiliary codes like 90785.
What is Code 90791?
90791 is a code for psych eval without medical services, most commonly used by those in the social and behavioral stratum of professional services, i.e., psychologists, social workers, and licensed professional counselors.
Characteristics:
· No medical auxiliary services or prescription management involved.
· Non-MD mental health professionals carry it out.
· A comprehensive review of an individual’s mental health history, along with current relevant symptoms and a mental status examination, is carried out.
Procedure code 90791 is the first code assigned throughout the psychotherapy process and is the basis upon which other subsequent codes (and thus payments) are authorized, making it essential for preliminary diagnosis and treatment decisions.
What is Code 90792?
Psychiatric eval with added medical services to previously mentioned 90792, this code indicates that medical services are available, hence available only to licensed medical professionals (MDs or DOs) able to prescribe medications.
Key Features:
· Comprises a medical examination and medication review.
· Quote this code only if the evaluation is done by a qualified healthcare professional, like a psychiatrist.
· Medically preoccupied with issues of physical wellbeing and incorporated medication into the broader multidisciplinary, intricate psychiatric assessment conducted in 90791.
90791 Reimbursement Rate
For the CPT code 90791, the set reimbursement value from Medicare is approximately $165.00.
This value serves as a national standard; however:
· Depending on their predetermined payment frameworks, private insurers might reimburse either more or less.
· Reimbursement rates may vary from state to state, and Medicaid rates may tend to be lower than Medicare.
Reimbursement Rate for 90792
Medicare reimburses approximately $196.55 for CPT code 90792.
· Private insurance and Medicaid may dispute these rates.
· Always verify reimbursement using payer-specific fee schedules or portals.
90791 CPT Code time
There are no specifically allocated minutes to CPT 90791, but it is expected to take between 60 to 90 minutes.
Findings with:
· Involvement of the hegemonic medical professional.
· Thoroughly detailed understanding of the patient’s medical biography.
· Gauge interview or document analysis.
90792 Time Requirements
Also, like 90791, 90792 is not specific, but within the range of 60 to 120 minutes is how long most evaluations are expected to take.
A substantial length of time is due to the extensive medical assessment and/or medication therapy management.
90791 Billing Guidelines
Quote this code only for psychiatric diagnostic evaluation without medical services
Who can bill:
The registered non-physician mental health professionals such as psychologists, social workers, and licensed counselors.
Do not bill 90791:
· More than once per episode of care, unless there exists medical justification.
· On the same day as E&M services by the same provider.
Documentation must include:
· Outpatient Mental Health Services: patient’s Psychiatric history and psychosocial history.
· The entire Mental Status Examination (MSE).
· Based on DSM-5 or ICD criteria, provide impression, diagnosis, with initial treatment recommendations.
Guidelines for Billing 90792
Includes medical services, unlike 90791.
Who can bill:
Legally qualified medical practitioners such as Psychiatrists (MD/DO) or other Nurse Practitioners and Physician Assistants who, by law, are allowed to provide psychiatric services.
Documentation must include:
· All elements of 90791 (history, MSE, diagnosis). A Medical Assessment (review of systems, physical health issues).
· Medication assessment and treatment plans, if relevant.
Summary Table: CPT 90791 vs 90792
| Feature | CPT 90791 | CPT 90792 |
| Description | Psych diagnostic eval without medical services | Psych diagnostic eval with medical services |
| Reimbursement (Medicare, 2023) | ~$165.00 | ~$196.55 |
| Provider Type | Non-MD mental health professionals | Psychiatrists, MD/DO, or NPs with a psychiatric specialty |
| Typical Duration | 60–90 minutes | 60–120 minutes |
| Includes Medication Assessment | No | Yes |
| Re-Evaluation | Possible if justified | Possible if medically necessary |
| Can be billed with E/M codes | No | No |
| Key Documentation | History, MSE, diagnosis | History, MSE, diagnosis + medical/medication evaluation |
Related CPT Codes for 90791 and 90792
To denote added intricacy or extra work done, a particular add-on CPT may be attached:
90785 CPT Code Description:
Interactive complexity: When communication is made difficult due to emotional, behavioral, or developmental issues.
90833 CPT code description:
· This is a 30-minute add-on that may be billed with E/M services and 90792.
· It is not a separate billable code; it must be used with another primary service code.
90836 CPT Code description:
· Psychotherapy 45 minutes add-on.
· Like 90833, this is used in conjunction with an E/M code like 90792 when therapy and medication management occur concurrently.
If you’re a mental health provider looking to understand how 90833 integrates with E/M services or wondering when to use codes like 90832 vs 90833, this guide on psychotherapy CPT codes might be especially helpful. It’s a practical read for those billing therapy sessions alongside psychiatric evaluations like 90791 and 90792.
Psychological testing: CPT codes 96116 and 96131.
· 96116 CPT Code: Neurobehavioral status exam, commonly lasting 30 minutes. Frequently applies to cases of brain injury or dementia, which involve administering neuropsychological tests.
· CPT Code 96131: A clinician providing feedback that accompanies test results through a detailed report and comprehensive assessment of the actual test results.
These should not be confused with 90791 or 90792, but may be considered several mental health evaluation frameworks.
Best Practices for Billing 90791 and 90792.
Check Eligibility:
The provider’s registration must match the service billed for 90791 and 90792.
Use of Modifiers:
Assign modifier AF to psychiatrists (90792), AH to psychologists (90791), and AJ to social workers.
Document Issues:
For a 90792 billed service, the record must include history, mental status exam, diagnosis, and any medical evaluation as applicable.
Avoid Same-Day Conflicts:
Don’t claim reimbursement for 90791 and 90792 alongside other E/M codes by the same provider on the same day unless there are payer-specific overrides.
Conclusion
In mental health care, proper CPT coding clause the conduct policy, and reimbursement policies help balance compliance and appropriateness of reimbursement of the funds. The primary distinction between 90791 and 90792 rests on the type of provider’s supervision, along with the presence of supplementary medical activities such as prescriptions traditionally offered during the diagnosis.
With proper application of add-on codes and knowledge of psychological testing codes such as 96116 and 96131, providers can ensure full representation of their services and appropriate reimbursement.
Ensuring consistency with proposed revisions on CPT coding, like changes of reimbursement for 90971 CPT code and guidelines for 90792, and partnering with a professional billing team opens possibilities to maintain compliance with policy and optimization, and makes the reimbursement process easy.