Did you know that over a quarter of denials of medical claims in the U.S. are due to errors in eligibility and insurance verification? It can take months of payment delays caused by a single incorrect move in the VOB in Medical Billing process, or even result in zero income. This is the reason why intelligent healthcare providers consider VOB as an unnegotiable component of their billing process.
At Providers Care Billing LLC, we have witnessed the potential of effective insurance eligibility verification to generate more cash flows, reduce denials, and create trust with the patients. This guide considers what VOB is, why it is important, how it can be integrated into contemporary billing processes, and how the assistance of professional billing can safeguard your revenue.
What is VOB ( verification of benefits) in Medical Billing?
Verification of Benefits in medical billing is a procedure that refers to the confirmation of insurance coverage of a patient prior to service. It informs the provider of the insurance payment, the amount to pay by the patient, and the need for prior authorization.
In simple terms, VOB insurance verification provides answers to such important questions as:
- Is the patient’s policy active?
- Is the service covered?
- What are co-insurance, co-pay, and deductibles?
- Is pre-authorization necessary in the plan?
Lack of adequate insurance verification during the medical billing process exposes the providers to unpaid bills, compliance issues, and dissatisfied patients. That’s why it is a foundational step in our professional medical billing services.
Understanding VOB in Medical Billing
Billing workflow commences much earlier than the billing claim. Clean claims, quick reimbursement, and reduced claims disputes would be based on insurance coverage verification. Read more about In-House vs Outsourced Medical Billing: What’s Better for Therapists?
You get when the insurance check is properly performed:
- Accurate claims
- Faster payments
- Proper patient accountability.
- Minimized revenue loss
We incorporate VOB in all phases of revenue cycle management (RCM) at Providers Care Billing LLC.
The VOB Process in Medical Billing: Step-by-Step
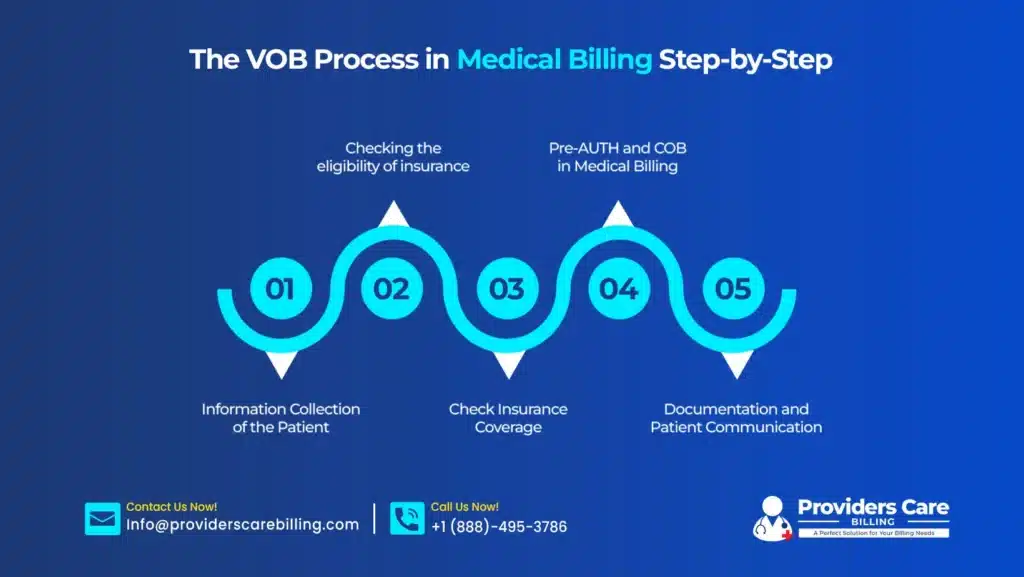
Step 1: Information Collection of the Patient
Verification of patients begins with accurate patient information:
- Insurance carrier name
- Policy number
- Group number
- Date of birth
- Subscriber information
A single misplaced digit would destroy the whole verification procedure.
Step 2: Checking the eligibility of insurance
The second step is the confirmation of billing specialists:
- Policy activity (present or not)
- Effective and termination dates.
- Network participation
This measure prevents coverage denials due to inactive or lapsed coverage.
Step 3: Check Insurance Coverage
The heart of VOB. Providers check:
- Covered services
- Visit limitations
- Deductibles
- Co‑pays
- Co‑insurance
- Out‑of‑pocket maximums
Proper coverage verification will make the providers aware of what will be reimbursed.
Step 4: Pre-AUTH and COB in Medical Billing
There are numerous plans that should be approved in advance. During this phase, billing personnel check the following:
- Pre-authorization conditions.
- Referral rules
- Coordination of Benefits (COB) when there is more than one insurance policy.
This step is usually not followed, which leads to automatic rejection of claims.
Step 5: Documentation and Patient Communication
The verified information is recorded in the system. The patients are informed in advance about:
- Projected out-of-pocket expenses.
- Payment expectations
- authorization requirements
Openness generates trust and enhances collections.
A single multi-specialty clinic contracted Providers Care Billing LLC due to frequent rejections. We discovered that their insurance check was not quite steady. Following an ordered VOB process, the clinic reduced denials by 32%, improved cash flow in the 60-day period, and increased scores in patient satisfaction. Healthcare providers offering medical billing services in New Jersey can achieve similar results by strengthening their verification process.
VOB vs EOB vs COB in Medical Billing
VOB, EOB, and COB are similar terms that have different uses in a particular phase of medical billing.
VOB, or Verification of Benefits, occurs before the delivery of services. It verifies insurance cover, eligibility, or services covered, deductibles and co-payments, and the prior authorization requirement of a patient. Doing the correct VOB helps avoid denial of claims and unforeseen balances for patients.
EOB, or Explanation of Benefits, is a document that is dispatched when an insurance company has handled a claim. It gives a description of the adjudication of the claim, such as the allowed amounts, payments, patient responsibility, and any denial reasons. EOB enables the providers to compare the anticipated and actual reimbursement.
In a case where the patient has more than one insurance plan, COB is the term applied. It will determine which is the primary and which is the secondary insurer, and claims will be properly billed. Proper handling of COB eliminates delays in payments and overpayments.
The combination of VOB, EOB, and COB generates a smooth and accurate billing process that begins with the correct verification process, transitions to proper claim processing, and concludes with proper reimbursement.
Importance of VOB in Medical Billing
- Reduces Claim Denials
Proper checking of insurance eligibility reduces claims refusals by establishing the existence of inactive policies, uncovered services, and authorizations at the earliest stages. With benefits confirmed in advance, claims are properly submitted on the first attempt, and payments are quickened, and cash flow is strengthened.
- Improves Cash Flow
Benefits verification involves transparency of costs. Patients are given the initial information on deductibles, copays, and coinsurance. This decreases the number of surprise bills, enhances satisfaction, and generates trust- eventually increasing cash flow.
- Improves Patient Experience
Verification of benefits (VOB) also provides correct reimbursements and a vibrant revenue cycle. Checking insurance details before service makes the responsibilities of the payer and patient very visible to the provider and thus makes the experience of all parties in a seamless manner.
- Ensures Compliance
Adequate verification is in line with CMS and payer guidelines. It helps to comply with the rules, reduce audit risk, and guard against the penalties of non-compliance affecting revenues.
Common Challenges in the Health Insurance Verification Process
The usual problems in the verification process of the Health Insurance. Although significant, VOB is usually not properly handled due to:
- Manual verification delays
- Complex insurance policies
- Frequent payer rule changes
- Inaccurate patient data
- Limited staff training
That is why the difference can be seen in outsourcing to such specialists as Providers Care Billing LLC.
How Providers Care Billing LLC Helps
We do not just check insurance, but protect your revenue. Our VOB/ Insurance Verification Services Involve:
- Instant verification of eligibility for insurance.
- Checking coverage in detail.
- The authorization and referral management.
- Reconcilement and follow-ups of Explanation of Benefits (EOB)
- adherence to billing updates every year.
Our company keeps up with annual coding updates, payer regulations, and CMS regulations; you do not.
Are you ready to stop claims denial and receive payment more quickly? Let Providers Care Billing LLC deal with your VOB with accuracy, compliance, and care.
Contact us now with a free billing consultation. Attend to patients, and we will take care of the insurance verification.
Final Thoughts
VOB is now necessary in the modern billing setting where there is a high degree of complexity and financial accuracy, compliance, and patient trust. Quality verification will decrease denials, accelerate reimbursements, and reinforce the whole procedure. Providers Care Billing LLC offers experienced billing services, which have enabled providers to secure their income and concentrate on providing quality care to patients without the bother of making billing payments.
Frequently Asked Questions
What does VOB mean in medical billing?
VOB checks the insurance coverage and benefits, and the financial responsibility of the patient, before the services are delivered.
What is the significance of checking the eligibility of insurance?
It will stop claims denials, make bills accurate, and allow providers to receive patient responsibility at the point of care.
What is the difference between VOB and EOB in medical billing?
VOB ensures coverage and before services; EOB reports how the claim was handled subsequently.
What is COB in medical billing?
COB comes into effect in instances where a patient has more than one insurance plan to determine how the payment order should be made to ensure that there is appropriate and prompt reimbursement